A cutting-edge approach known as normothermic regional perfusion (NRP) is allowing transplant teams to explore a much broader range of organ donors.
Traditionally, heart and liver transplants are performed using donors categorized as “brain-dead.” These donors no longer have brainstem reflexes, yet they maintain function in their hearts and other organs.
Although this donor pool has been ideal for securing usable organs, the availability of these organs isn’t enough to meet a growing need as heart and liver failure cases rise across the country.
A cutting-edge approach known as normothermic regional perfusion (NRP) is allowing transplant teams to explore a much broader range of organ donors — and early cases in the U.S. show promising results.
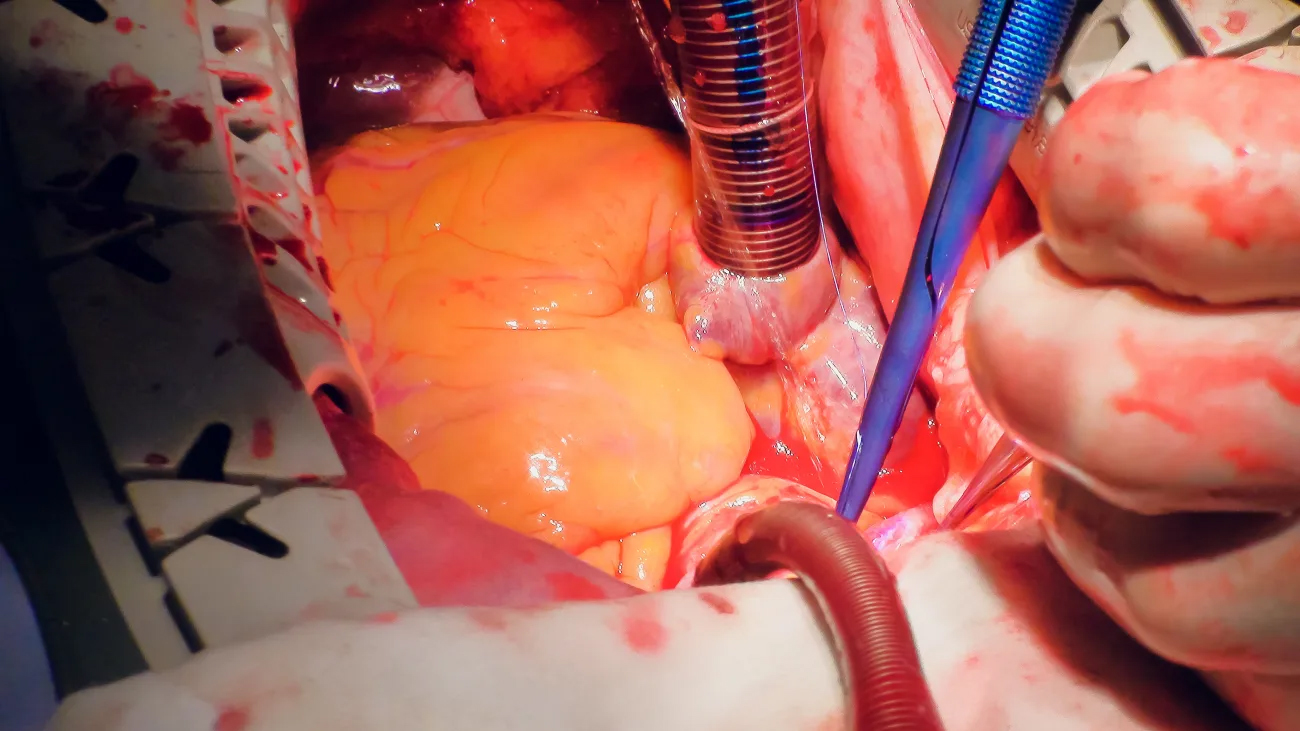
Perfusing the heart after circulatory death
In June 2023, Raymond Lee, MD, a cardiac surgeon at the USC Transplant Institute, part of Keck Medicine of USC, used the NRP technique to successfully transplant a heart into a 62-year-old patient with non-ischemic cardiomyopathy.
With NRP, surgeons transplant organs donated after circulatory death rather than brain death. These donors have experienced catastrophic neurological injuries but are not labelled brain-dead because they still maintain some reflexes.
“When the breathing tube is removed and the patient has cardiac arrest, somewhere between five to 10 minutes can pass beyond brain death before we can declare circulatory death,” Lee said. “We’re then able to perform an NRP heart procurement.”
Immediately after circulatory death, Lee opened the donor’s chest, placed the body on cardiopulmonary bypass and drained all the blood from the heart. He and his team then began perfusing the body while cutting off blood flow to the brain.
“We watched the heart come back to see if it was usable again after the cardiac death,” Lee said. “Once we saw that it was, we started preparing our recipient.”
Lee proceeded with transplanting the heart into the 62-year-old recipient at Keck Hospital of USC. The patient was discharged from the hospital about a month later in good condition.
Liver procurement from NRP donor
Using the same NRP donor that Lee’s heart transplant team perfused, a Keck Medicine liver transplant team also performed a successful transplant.
The recipient, who was experiencing liver failure, had been on the transplant list for less than a year.
American transplant teams have traditionally avoided NRP livers because of the stress placed on abdominal organs in the period after circulatory death.
However, with Lee’s perfusion, the donor heart quickly reestablished warm, oxidized blood flow to the liver.
“It really resuscitated the organ,” said Aaron Ahearn, MD, the Keck Medicine liver transplant surgeon who performed the procedure. “It allowed the liver to recover before it had to go on ice.”
Additionally, Ahearn and his team targeted a recipient they assessed would do well with an organ that had undergone the added stress.
The recipient was farther down on the transplant list than most recipients from brain-dead donors — and therefore healthy enough to endure it.
“The organ undergoes one major stress in the procurement process,” Ahearn said. “You can’t then put it into somebody who’s severely ill to the level of needing treatment in the ICU.”
With these guidelines in mind, Ahearn’s transplant was a success.
“This organ has the potential to last the recipient for the rest of his life — 40 to 50 years, potentially,” Ahearn said. “With continued follow-up and ongoing immunosuppressant medication, we consider him cured of his liver disease.”
‘The future of transplant’
According to Lee and Ahearn, the NRP technique offers transplant surgeons the chance to expand opportunities for patients in need.
“It’s potentially an organ pool that could be much larger than the traditional pool,” Ahearn said. “Many more people die in a fashion consistent with cardiac death than with brain death.”
In August 2023, the heart transplant team performed their second successful NRP transplant at Keck Hospital.
Their partnership with the abdominal organ transplant teams in the USC institute allows greater collaboration for future liver and kidney transplants as well.
“NRP allows us to take organs that were previously challenging and marginally unsafe to use and brings them to the safety level of our standard transplants,” Ahearn said. “I think this is the future of transplant.”
USC Transplant Institute
The USC Transplant Institute team takes a complete approach to caring for transplant patients and living organ donors. We make sure your patients have a team of experts on their side every step of the way, from evaluation to recovery.
Topics
